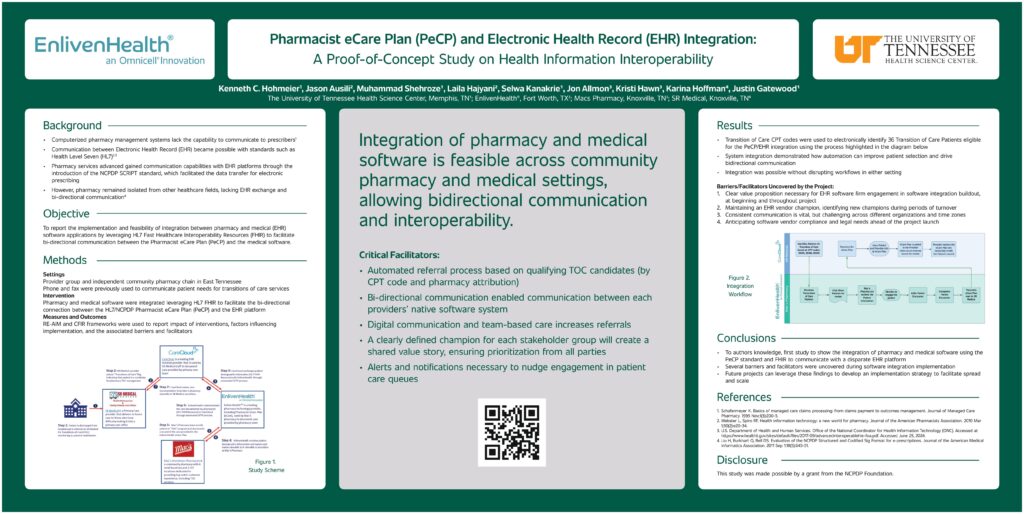
EnlivenHealth® and the University of Tennessee Health Science Center partnered on a proof-of-concept study made possible by grant funding from the National Council for Prescription Drug Programs (NCPDP) Foundation. The research found that integration of pharmacy and medical software is feasible across community pharmacy and medical settings, allowing bidirectional communication and interoperability.
Click the poster below for a larger version.
Addressing the Disconnect
Historically, computerized pharmacy management systems have lacked the capability to communicate with prescribers.1 Interaction between Electronic Health Record (EHR) systems became possible with standards such as Health Level Seven (HL7) and support from the formation of the Office of the National Coordinator for Health Information Technology.2,3 Pharmacy services gained communication capabilities through the introduction of the NCPDP SCRIPT standard, which facilitates the data transfer with EHR systems for electronic prescribing. However, pharmacy has largely remained isolated from other healthcare fields, lacking EHR exchange and bi-directional communication.4
Integrating Pharmacy & Medical Software
This objective of this study was to report the implementation and feasibility of integration between pharmacy and medical (EHR) software applications. In doing so, the study team recruited a provider group and an independent community pharmacy chain in East Tennessee. While both groups had an existing relationship collaborating on transitions of care (TOC) services, they resorted to phone and fax to communicate patient care needs prior to this project. The primary intervention entailed integrating the pharmacy and medical software, leveraging HL7 FHIR to facilitate the bi-directional connection between the HL7/NCPDP Pharmacist eCare Plan (PeCP) and the EHR platform. By employing the Reach Effectiveness Adoption Implementation (RE-AIM) and the Consolidated Framework for Implementation Research (CFIR) frameworks the study reported the impact of interventions, factors influencing implementation, and the associated barriers and facilitators to success.
Opening a Pathway for Bi-Directional Communication
The study results highlighted the referral process, which used TOC Current Procedural Terminology (CPT) codes to electronically identify 36 eligible patient candidates. The system integration demonstrated how automation can improve patient selection and eliminate error prone manual processes, while opening a new pathway for bi-directional communication. In addition, technology development enabled the integration to happen without disrupting workflows in either setting.
The video below demonstrates the workflow diagram and example screenshots of each vendor’s systems help to visualize the bi-directional exchange of information.
Breaking Through the Barriers
Key barriers and facilitators were also uncovered by the project. First, it was found that a clear value proposition is necessary to ensure EHR vendor engagement before, during, and after the software integration development phase. Maintaining a champion on the vendor side and quickly identifying new champions during periods of turnover was another facilitator of success. In addition, it was found that consistent communication throughout the project was vital but proved to be challenging across different organizations and time zones. Finally, anticipating software vendor compliance and legal needs ahead of product launch is crucial to achieving the goals of the project.
Conclusion
In closing, this study represents the first research project (to the author’s knowledge) to show the direct integration of pharmacy and medical software using the PeCP standard and HL7 FHIR to communicate with a disparate EHR platform. Several barriers and facilitators were uncovered during the project that will enable future projects of this nature to leverage these findings to develop an implementation strategy to facilitate greater spread and scale.
- Schafermeyer K. Basics of managed care claims processing: from claims payment to outcomes management. Journal of Managed Care Pharmacy. 1995 Nov;1(3):200-5.
- Webster L, Spiro RF. Health information technology: a new world for pharmacy. Journal of the American Pharmacists Association. 2010 Mar 1;50(2):e20-34.
- U.S. Department of Health and Human Services. Office of the National Coordinator for Health Information Technology (ONC). Accessed at https://www.healthit.gov/sites/default/files/2017-09/advancedinteroperablehie-foa.pdf. Accessed June 25, 2024.
- Liu H, Burkhart Q, Bell DS. Evaluation of the NCPDP Structured and Codified Sig Format for e-prescriptions. Journal of the American Medical Informatics Association. 2011 Sep 1;18(5):645-51.
