Pharmacy Transformation Delivered
Trusted by leading pharmacies to help improve patient experiences and outcomes, streamline adherence and clinical workflows, optimize financial performance, and drive business growth through innovative software and services.
Trusted by more than 44,000 of the leading pharmacies.
Tailored Solutions Helping Pharmacies Overcome Challenges and Scale Efficiently
Disconnected Patient
Interactions

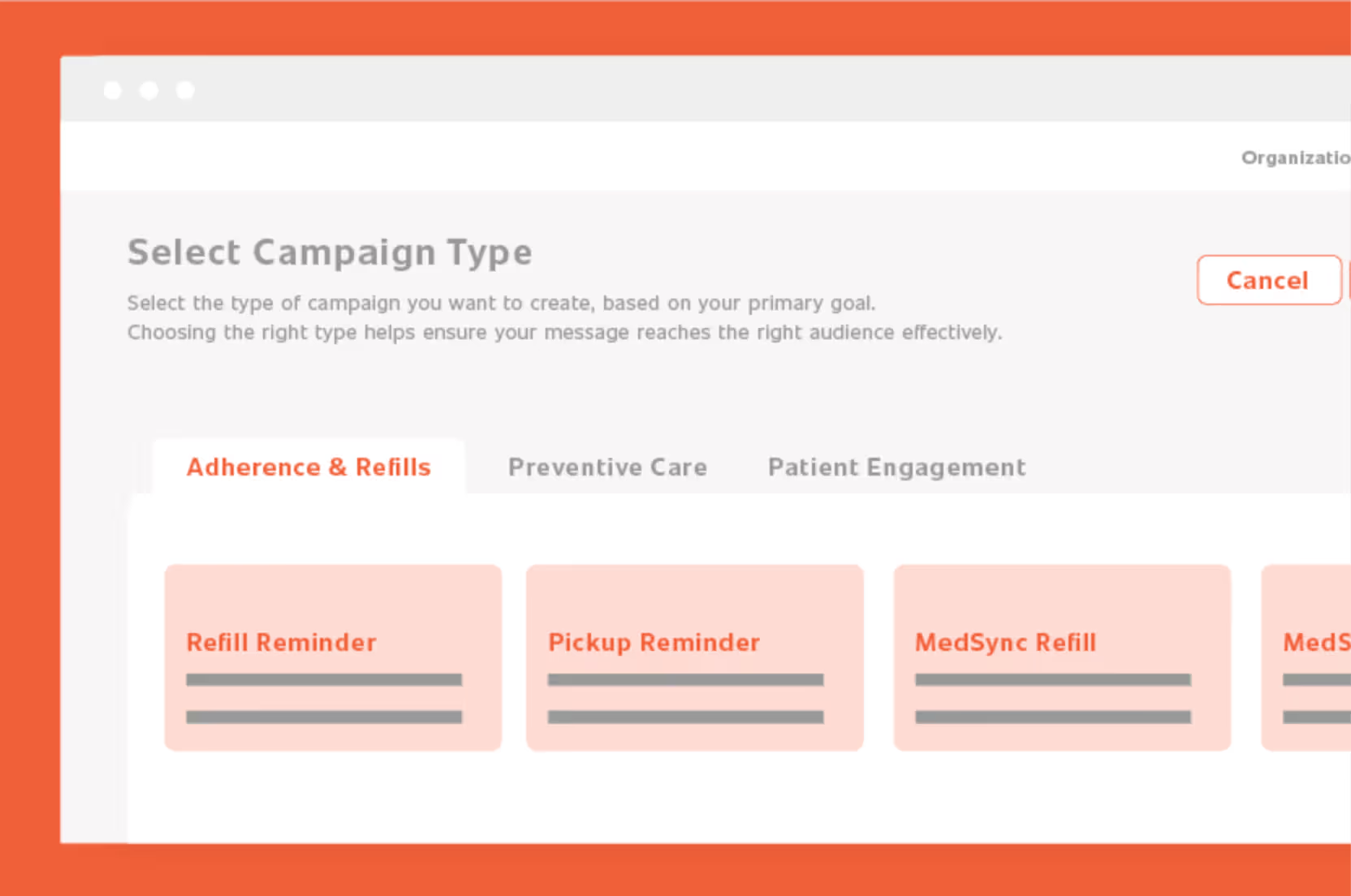
Enhance Patient Pharmacy Connections
Strengthen patient-pharmacist relationships through seamless connectivity. EnlivenHealth’s engagement solutions make your pharmacy more accessible while simplifying and streamlining outreach—transforming routine interactions into meaningful connections that improve both patient loyalty and outcomes.
Clinical Care
Barriers

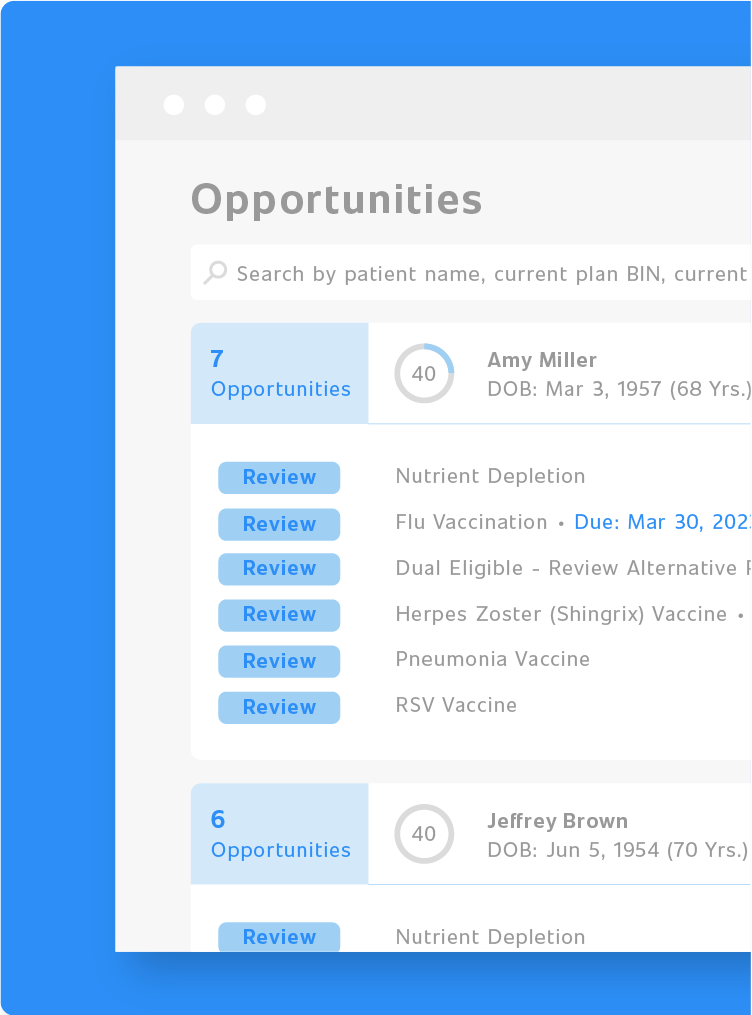
Expand Clinical Services with Ease
Transform manual, complex workflows into an efficient clinical experience. EnlivenHealth’s clinical solutions streamline medication dispensing, automate routine tasks, and support clinical service expansion—enabling your pharmacy to deliver exceptional patient care while maximizing operational efficiency.
Increasing Financial
Pressures

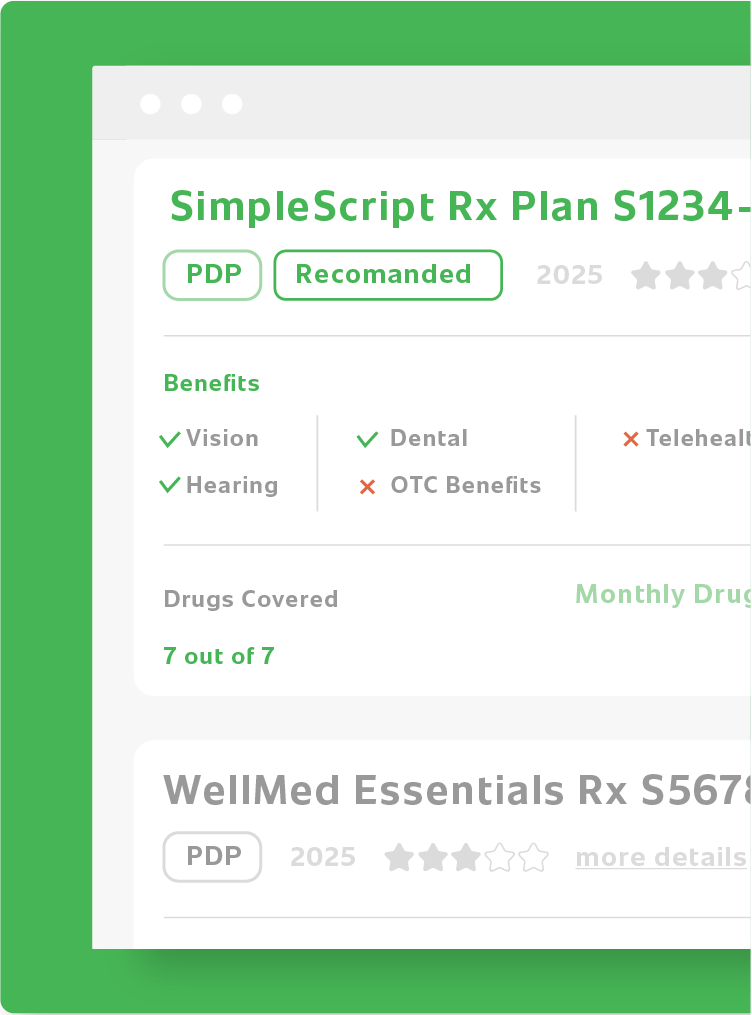
Strengthen Financial Performance
Navigate today’s tough financial landscape with confidence. EnlivenHealth’s financial solutions streamline revenue cycles, optimize reimbursements, and enhance operational efficiency—giving your pharmacy the tools to maintain profitability while delivering exceptional patient care.
Underperforming
Revenue Streams

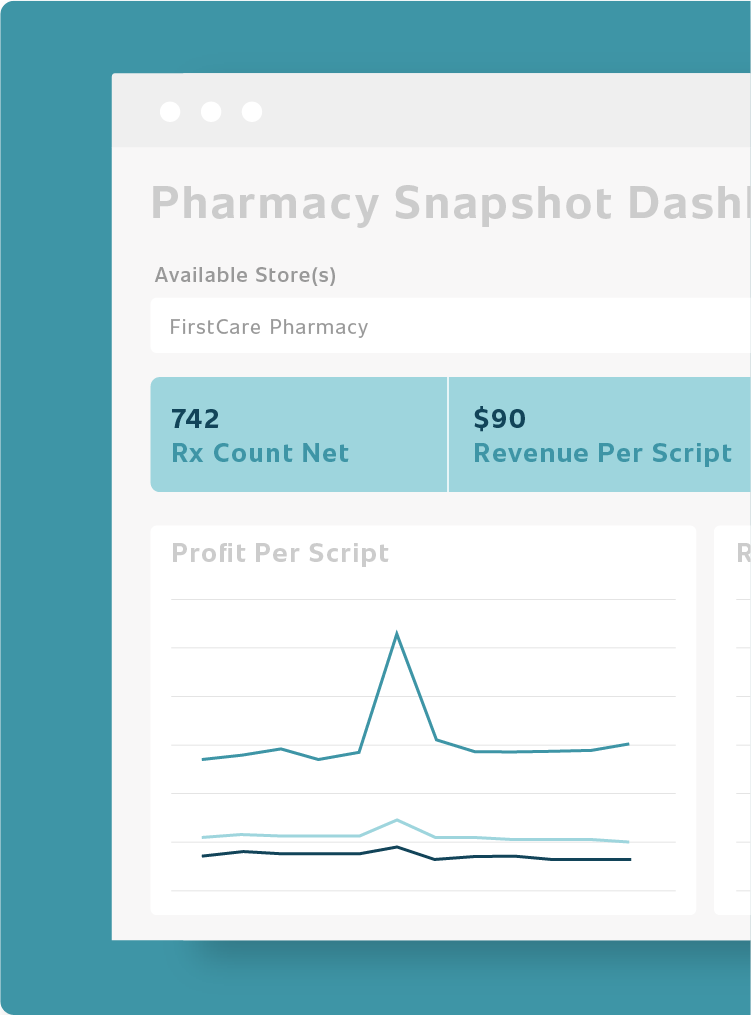
Discover Data-Based Growth Opportunities
Unlock hidden pharmacy potential through data-driven insights. EnlivenHealth’s business intelligence solutions uncover revenue and adherence opportunities while measuring pharmacy performance—transforming complex pharmacy data into actionable strategies that boost profitability and operational excellence.
Tailored Solutions Helping Pharmacies Overcome Challenges and Scale Efficiently
Passionate About Delivering Insights & Outcomes for Community Pharmacies
Our solutions deliver tangible outcomes for pharmacies of all sizes—boosting revenue, enhancing medication adherence, and strengthening patient-pharmacy connections across thousands of locations nationwide.